Hypervolaemia
We have now covered hypovolaemia as a cause of hyponatraemia, and the mechanism by which it occurs. You may already be aware that hypervolaemia can also be a cause of hyponatraemia.
The surprising thing, however, is that the mechanism is exactly the same as in hypovolaemia. This is the reason that we stressed that the body needs to perceive a severe hypovolaemia for the usual role of the osmolality regulation system to be diverted from osmolality to volume.
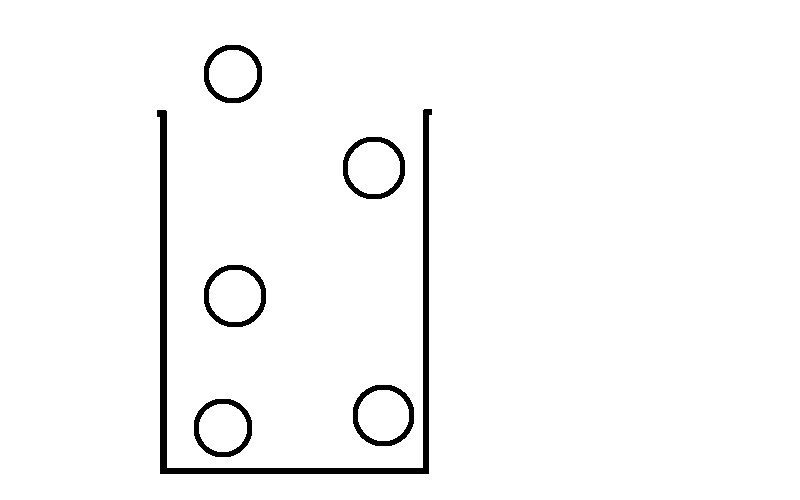
In many cases of fluid overload, this is exactly what happens:
- Some initial trigger disrupts the body's equilibrium and increases volume status to a critical level.
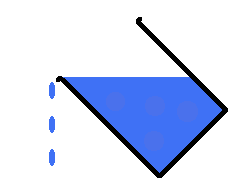
- The body enters a state in which total body volume is high, but intravascular volume is low, and so the kidneys sense a reduced perfusion and think that this can be solved by increasing volume.
- It increases activity of the RAAS and other mechanisms which increase volume.
- This worsens the initial problem, and the cycle repeats.
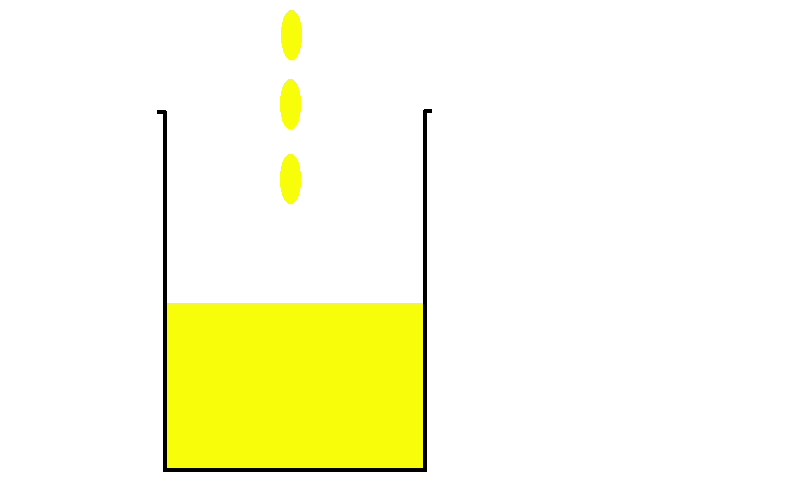
At some point in this cycle, the perfusion that the kidneys perceive may be so low that it initiates the same backup system which we have seen happens in hypovolaemic states, i.e. ADH is secreted in a last resort attempt to increase volume (even if in this case, whole body volume is already very high). This then increases volume by increasing pure water content, which reduces sodium concentration and thus reduces osmolality.